1. Why is it recommended that baby should be given only mother’s milk and not any other milk?
Breastmilk is a natural complete food for the baby. All mammals produce milk that is species specific for their own offspring like Human milk is for human baby while cow’s milk is for her calf.
Breastfeeding offers many advantages to mother-infant pair. These are listed below. Baby and mother will not get these benefits if animal milk or formula is used for feeding.
Advantages offered by Breastmilk and Breastfeeding
For the baby:
- All the nutrients are in proper proportion for optimal growth and development
- Easily digestible
- Germ free as it is transferred directly from the mother to the baby
- Provides immune factors which provide protection against infections e.g. pneumonia, diarrhoea etc.
- At right temperature
- Makes child more intelligent
- Protection against asthma and allergies
- Protection against obesity, hypertension, heart disease and diabetes in later life
- Decreased risk of some cancers
- Stronger Mother – Infant bonding
For the mother:
- Loses fat through breastmilk. Helps her to get back in shape (to be complemented with exercises and avoidance of excessive fat intake)
- Decreased risk of breast, ovarian and uterine cancers
- Helps to delay next pregnancy; but the mother should not depend on this (LAM – Lactational Amenorrhea Method) as the sole method of contraception (To consult doctor six weeks post-delivery).
- Early expulsion of placenta
- Uterus contracts faster to pre-pregnancy state
- Decreased post-delivery bleeding
- Convenient and requires no preparation
- Protects from post-menopausal osteoporosis.
- Free of cost. Breastfed babies fall less sick. Hence family saves on medical expenses.
- Declining breastfeeding rates would increase the need for animal milk. This can damage the environment. Hence breastfeeding is environment friendly
Note: Breastfeeding is advantageous not only for the mother and baby but also for the overall development of the society and the nation.
2. How should mother prepare for breastfeeding during pregnancy? Should she take some special care of breasts and nipples?
Baby needs to be exclusively breastfed till the end of 6 months. Both mother and family need to get psychologically geared up for this task. The family routine changes after child’s birth. Extra effort and extra hands are required to meet the increased workload. All family members should provide encouragement, adequate time, and supportive environment for breastfeeding.
Everybody should get to know scientifically correct information on advantages of breastfeeding, IYCN recommendations, positions, attachment, and commonly encountered problems. A pregnant mother can immensely benefit by observing another mother breastfeed and sharing experiences.
Breasts and nipples undergo natural changes as the pregnancy advances. The nipples which initially appear smaller become optimally fit for feeding by the time of delivery. The mother should not worry about the size of the breasts because milk production does not depend on it. The breast size varies due to differences in amount of fat. Amount of milk producing glandular tissue is almost same in all the mothers.
Proper clothes that facilitate breastfeeding need to be kept ready. Sari-Blouse, shirt, or gown (full front opening) is best suited for this purpose.
3. When should breastfeeding begin after delivery and how?
Soon after delivery the baby should be shown to the mother. Mother should be promoted to kiss and cuddle the baby and hold the baby in close skin to skin contact (in about 5 min.) in Breast Crawl Position. This helps the baby to initiate breastfeeding in one hour. The Breast Crawl Video (breastcrawl.org) will guide you to implement this recommendation After Caesarean, the mother can initiate breastfeeding with the help of care givers as soon as she feels ready, preferably within four hours of birth.
Following are the benefits of early initiation.
- Baby is very alert and eager to breastfeed in the first hour after delivery.
- The child remains warm being in close touch with the mother
- Risk of infections is reduced
- Ensures short term and long-term breastfeeding success (Total Duration)
- Post-delivery bleeding (Post-partum hemorrhage) decreases
- A strong emotional bond begins to develop between the mother and the baby.
Note: The first skin-to-skin contact should continue till completion of the first breastfeed.
4. Mother does not produce milk for first few days after delivery. What should be fed to quench baby’s thirst and hunger during this period?
Even though the mother does not produce milk during the first two- or three-days post-delivery, she produces a yellow fluid known as colostrum. Though less in quantity, it is enough to meet baby’s needs. Following are the benefits of colostrum:
- Rich in antibodies (immunity) and protects the baby against infections. Hence it is the first vaccine for the baby.
- Helps the baby to pass her first stool (meconium). This helps to reduce the severity of physiological (normal) jaundice.
- Helps to complete maturation of the intestines
- Rich in vitamins A and K
The relatives and health care providers should motivate the mother to give frequent skin to skin contact and breastfeed as soon as the baby shows the desire to do so. This ensures that the baby gets good quantities of colostrum. Some children cry little more during this period. But one should avoid the temptation of giving any milk or fluids (water, glucose, honey etc.) because this increases the risk of infection. Instead, the mother should focus on frequent skin to skin contact and breastfeeding (at least 8-10 times in 24 hours).
5. Is it appropriate to follow the tradition of giving honey, sugar water, etc. to the baby before the first breastfeed (Pre-Lacteal feeds)?
Traditionally, sometimes the baby is fed some fluid before the first breastfeed or during first three to five days of life (before the mother starts producing mature milk). This is known as ‘Pre-lacteal feed’. This custom is inappropriate because it increases the risk of infection. This pre-lacteal feed may decrease the baby’s eagerness to suckle at the breast. Thus, the first and the subsequent breastfeeds may get delayed. This may lead to breastfeeding failure.
6. Where should the child be kept after delivery?
The child should be kept close to the mother (bedding in). It is not advisable to keep the baby in a cradle or on a separate bed. In some maternity homes, all newborn babies are kept together in a separate room. This is a wrong practice. The word ‘rooming in’ means that the mother and the baby are kept in the same room. The benefits of ‘bedding in’ are as follows:
- It promotes demand feeding
- The baby remains warm
- Risk of infection is reduced
- Helps let-down of milk
- Helps to develop a stronger emotional bond between the mother and the baby.
7. How frequently and how long should the child be breastfed?
It is necessary to feed the baby more frequently during the first 1-2 weeks (at least 10 times in 24 hours). That means that the baby should be promoted to breastfeed every 1.5 – 2 hours. At this point of time, the baby may be already hungry or may still be sleepy.
A hungry baby will show early feeding cues (This may occur before 1.5-2 hours after the last feed) Every mother and family should be aware of these cues
Early Feeding Cues (Indication or signs that the baby is hungry)
- Restlessness
- Eye movements, as if the bay is looking for the mother
- Soft cooing or sighing sounds
- Rooting (Mouthing movements with head turning as if trying to attach to the breast)
- Sucking sounds
- Hand-to-Mouth movements
There is a myth that the baby should be fed only after crying. This is misleading. Crying is a late feeding cue and a crying baby does not breastfeed easily. Hence the baby should be fed as soon as the above early feeding cues are seen.
If the baby is sleepy then the mother should attempt to wake up the baby as follows:
Strategies to wake up a Sleepy Infant for feeding
- Remove blankets
- Remove clothes
- Change the infant’s loin cloth if soiled
- Place the infant skin-to-skin in Kangaroo Position (Infant placed on mother’s abdomen with head in between the breasts)
- Massage the infant’s back, abdomen, arms & legs
Only after child starts urinating frequently (more than 6 times in 24 hrs.) and starts gaining weight that the baby can be fed on demand. i.e. whenever the baby wants and as long as she wants (Still, the baby should be fed at least 8 times in 24 hours). This would usually occur at 1-2 weeks of age.
Very few babies demand feeds with a regularity of 2-3 hours. Some sleep during the day and keep their mothers awake at night. Some have exactly opposite schedule. Some children do not follow any definite timetable. Some babies sleep for a long time and then after waking up feed very frequently for many hours and also urinate frequently. All these patterns should be considered as normal. The mothers should adjust her daily routine to suit baby’s needs.
Some babies are fast feeders (finishing their breastfeed in 5 to 10 min.), while slow feeders may continue to suckle for as long as 30 to 45 min. Mother should feed on one side as long as possible because the milk which comes initially is rich in water & sugar (foremilk), while the milk which comes in the later part of the breastfeed is rich in fats (hind milk). It is necessary to feed the child frequently at night and there are no ill-effects associated with this. In fact, the mother produces more milk during the quiet hours of night. It is not mandatory for the mother to breastfeed in sitting position; she can also feed while lying down. She may find it more comfortable.
8. How should the mother hold the child while breastfeeding?
How baby suckles from the breast
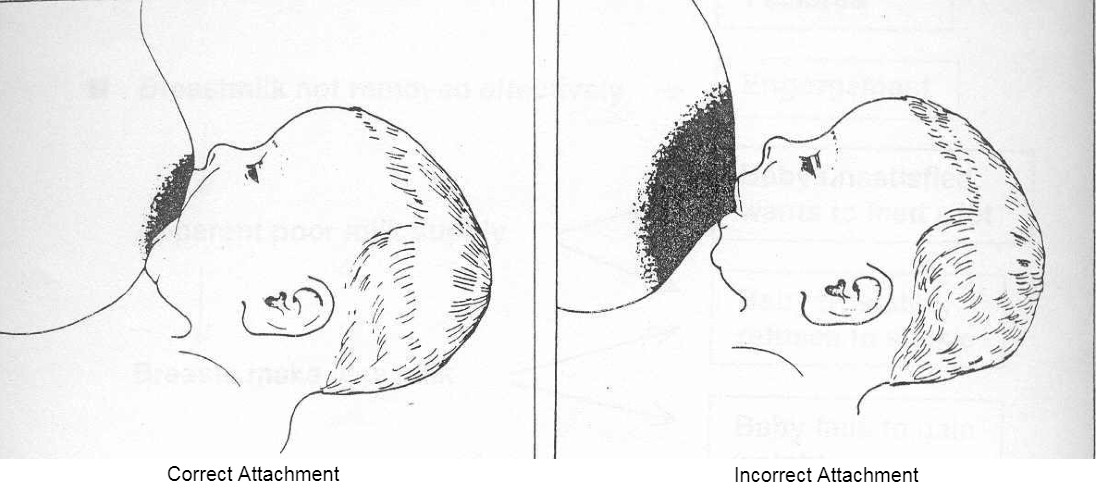
Baby’s Attachment
- Maximum possible areola inside the baby’s mouth (Lower portion more).
- Mouth wide open.
- Lower lip turned outward.
- Chin touches the breast.
Baby’s Position
- Turned towards the mother (Tummy to Mummy)
- Good skin to skin contact.
- Head & body in one line. (Ear, Shoulder and Hip in one line)
- Neck, back & buttocks well supported.
Mother’s Position
- Sitting comfortably with good back support
- Holding breast in big ‘C’ grip of hand
- Touches nipple to upper lip by bringing nipple in front of nose & gives mouthful of breast as soon as the baby opens the mouth widely
- Interacting with baby while feeding
Note: If child is more than one month old and it is certain that the baby is getting enough milk, it may not be wise to instruct the mother regarding attachment and positioning.
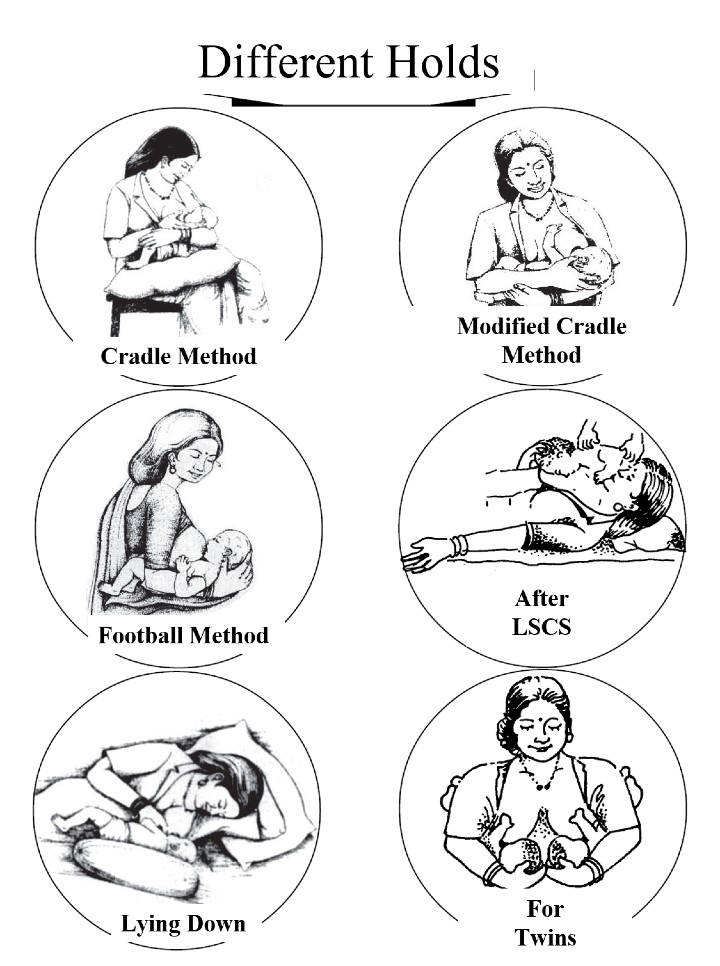
To see the different ways in which the mother can hold the baby refer to the diagrams of ‘Different Holds’ as follows
9. What is the cause of cracked / sore nipples? What is the remedy?
If the baby’s attachment to the breast is not as described above (Answer 8) then it causes cracked\sore nipples. The prevention / remedy is learning correct attachment. The mother should apply hind milk to the cracked/sore nipple and leave it open to the air for some time. Frequent washing of nipple and areola with soap and water can cause drying and cracks by removing the natural oily substance which normally covers this area. Routine once a day cleaning of the breasts during bath is enough. Nipple may get cracked at the base if the child is taken away abruptly from the breast while feeding. Hence if the baby must be removed from the breast, the mother should insert her little finger in baby’s mouth and detach the baby slowly.
Note: To avoid cracked/sore nipples mother should learn the proper technique of attachment right from the first breastfeed. Ensuring that mother does not feel pain while feeding confirms good attachment.
10. What should a mother do if breasts get hard and lumpy (engorgement)? What causes this?
The mother starts producing milk (i.e. mature milk) from three to five days after the delivery. Excessive production of milk or incomplete emptying of breast (Infrequent suckling or poor attachment) will cause heaviness, hardening and pain (engorgement). Engorgement restricted to a part of the breast will give a lumpy feel. Engorgement of the breast tissue which is normally present in the armpit will produce a lump there. Engorgement may sometimes be caused if the child has overslept and not fed.
Breasts become full and little heavy just prior to a breastfeed (Full Breasts). Breasts will start getting engorged if not emptied for some more time (Engorgement). Engorgement can be prevented by feeding the baby at regular intervals or by timely expression of milk. Hence it is essential that every mother knows this technique of expression. Unattended engorgement can lead to increasing pain, redness over a part of the breast and fever (Mastitis). If neglected, this may progress to pus formation (Breast Abscess).
11. How long should the baby be breastfed? When should water, gripe water, balkadu etc be given to the baby?
The baby should be given only breastmilk (Exclusive Breastfeeding) for the first six months of life. Even water is not necessary during this period. Breastmilk contains enough water to take care of baby’s needs even in summer.
It is unnecessary to feed the baby with traditional items like balguti, gripe water, balkadu multivitamin/mineral preparations etc. Feeding these items may cause frequent infections. These substances may make the child less eager to breastfeed either due to partial satisfaction of hunger or due to presence of sedating chemicals. Proper complementary foods should be started at the end of six months. However, breastfeeding should continue along with complementary foods at least till second birthday. Breastfeeding can be continued to some extent till the child is five years old because child’s immunity matures only by this age. Continued breastfeeding till this age reduces the risk of various infections.
12. How to know that the baby is getting enough breastmilk?
There are two gold standards to know if the baby is getting enough breastmilk; of this, one can be easily observed at home. If an exclusively breastfed baby is urinating at least 6-7 times in a day, i.e. in any 24-hour period, it implies that she is getting enough. One can draw the same conclusion if the child gains at least half a kilo, i.e. 500 grams every month. These two tests cannot be used for about a week or two after birth when breastfeeding is getting established. During the first 3-5 days the baby passes urine infrequently and a full-term newborn loses 7-8 % weight. Increasing urine output and weight after 3-5 days of birth indicate that the mature milk has come in and baby is getting it in good quantities. Baby regaining birth weight by 15th day of life has similar implications. Baby doubles her birth weight in about 5 months and triples in one year.
Many mothers complaining about less breastmilk would in fact report that the baby has frequent urination and a good weight gain. Mother of such a baby may feel that her milk is inadequate due to following reasons:
- If a child cries excessively it is always taken to mean that the mother is not getting enough milk. A baby may cry for many reasons other than hunger. A baby can express any discomfort only by crying out.
- Milk comes in between 3-5 days after delivery. This can sometimes cause heaviness and mild engorgement of the breasts. However, after a few days this heaviness passes off and breasts again become soft. Hence mother may feel that she is not getting enough milk.
- The child often sucks at fingers (mouthing); but this is quite common and does not necessarily imply that the baby is hungry.
- After breastfeeding is established in about a week, spontaneous dribbling of milk may occur for a few weeks from the other breast while the mother breastfeeds. This stops later.
- Babies grow faster during some periods (Growth Spurts). Babies feed frequently for longer periods during growth spurts.
Note: Frequent suckling (with correct attachment) makes more milk.
13. Should breastfeeding be stopped during mother’s illnesses?
It is not necessary for a mother to stop breastfeeding even if she is suffering from fever/cold/cough/vomiting/diarrhoea/and many other common illnesses and infections. Since the mother and the child live in the same environment and are in close contact, the child is usually infected by the time mother shows the symptoms. The child may have a shorter illness because it gets the antibodies (immunity) produced in the mother’s body through breastmilk.
14. Is it correct to enforce dietary restrictions on mother with the fear that some food substances can affect baby’s health?
Breastmilk is produced from blood. Composition of blood remains unchanged irrespective of what mother eats and so does composition of breastmilk. However, it is necessary that the mother takes a balanced diet and eats some extra food to support lactation. Routine tradition of giving ghee enriched sweet preparations to a breastfeeding mother would stand to reason only if she is undernourished, or else this would only contribute to making mother more obese. The mother should avoid eating outside food due to the risk of contracting an infection.
15. Is it all right to use a bottle for giving water or milk to a child?
It is always unsafe to use the bottle. The risk of vomiting and loose motions (acute gastroenteritis) and other infectious diseases is much higher in bottle fed babies. Since it is easier to feed from a bottle, the child may subsequently refuse to breastfeed (nipple confusion). While bottle feeding, child can accidentally aspirate milk (suck milk into lungs). This may endanger her life. It is always safe to use cup, katori-spoon or a glass to feed the baby.
16. How should a working woman combine work with breastfeeding?
Mother should try to take maximum possible maternity leave, major chunk of which should be enjoyed after delivery. Expressed breastmilk remains fresh for 6 hours at room temperature (4 hours in summer) and for 24 hours if kept in refrigerator (chiller compartment). The cold milk from the refrigerator should not be directly warmed over a flame. In summer, it should be allowed to come to room temperature or else it may be placed in a pot containing hot water. The working women should make use of this information. They can store the extra milk after each feed while at home or express and store milk at workplace if facilities permit (If these facilities are not available then mothers should periodically express milk and discard it to prevent engorgement and reduced milk supply). This stored milk can then be transported back home to be used next day. This stored milk can be fed to the child with cup (Katori) and spoon when mother is at work. If feasible, the mother should try to come home to breastfeed the child in between working hours or mother can carry the baby to workplace if crèche facilities are available. She should try to get transfer or a new job nearer to her house. If a mother breastfeeds her baby more frequently at night, the child will demand less during the day.
